Polycystic Ovarian Syndrome (PCOS) is a common but complex hormonal condition that affects women of reproductive age. It often shows up as irregular periods, weight struggles (especially around the middle), acne, or fertility challenges—but symptoms can vary widely.
With PCOS, your body has a harder time managing blood sugar, which can lead to increased belly fat, higher cholesterol, and a greater risk of type 2 diabetes and heart disease. PCOS doesn’t just affect physical health—it can also impact mental well-being, with higher rates of anxiety, depression, and disordered eating. Sleep issues and other conditions, like fatty liver disease or endometrial cancer, are also more common.
In this blog, we will share:
- The Role of Insulin Resistance
- The Best Diet for Managing PCOS
- How to Build a PCOS-Friendly Plate
- What Foods Make Your Symptoms Worse
- Lifestyle Strategies for Managing PCOS
- Movement Increases Insulin Sensitivity
- Sleep and PCOS Symptoms
- Stress and PCOS Symptoms

The Role of Insulin Resistance
One of the major drivers of PCOS symptoms is insulin resistance. Insulin is a hormone made by your pancreas that acts like a key, helping sugar (glucose) move from your bloodstream into your body’s cells where it can be used for energy. After you eat—especially foods with carbohydrates—your blood sugar rises, and insulin is released to help bring it back to a normal level. But in people with insulin resistance, the cells don’t respond properly to insulin’s signal. This forces the body to produce more and more insulin to get the job done.
Why is this so important when it comes to PCOS? High insulin levels can signal the ovaries to make more androgens (like testosterone), which can disrupt your menstrual cycle, make it harder to ovulate, and cause symptoms like acne, excess hair growth, and difficulty losing weight. Over time, it may also raise your risk for type 2 diabetes.
The good news is that insulin resistance can improve with targeted lifestyle changes. That’s where the Well Balanced method comes in—focusing on balanced meals (with protein, healthy fat, fiber, and colorful plants), joyful movement, sleep, and stress support. These simple steps can help your body respond better to insulin, reduce symptoms, and support hormone balance from the inside out. Let’s go over each one.
The Best Diet For Managing PCOS
A balanced, anti-inflammatory eating pattern—like the Well Balanced approach —remains one of the best strategies for managing PCOS. This eating style supports stable blood sugar, reduces insulin resistance, and promotes hormone balance.
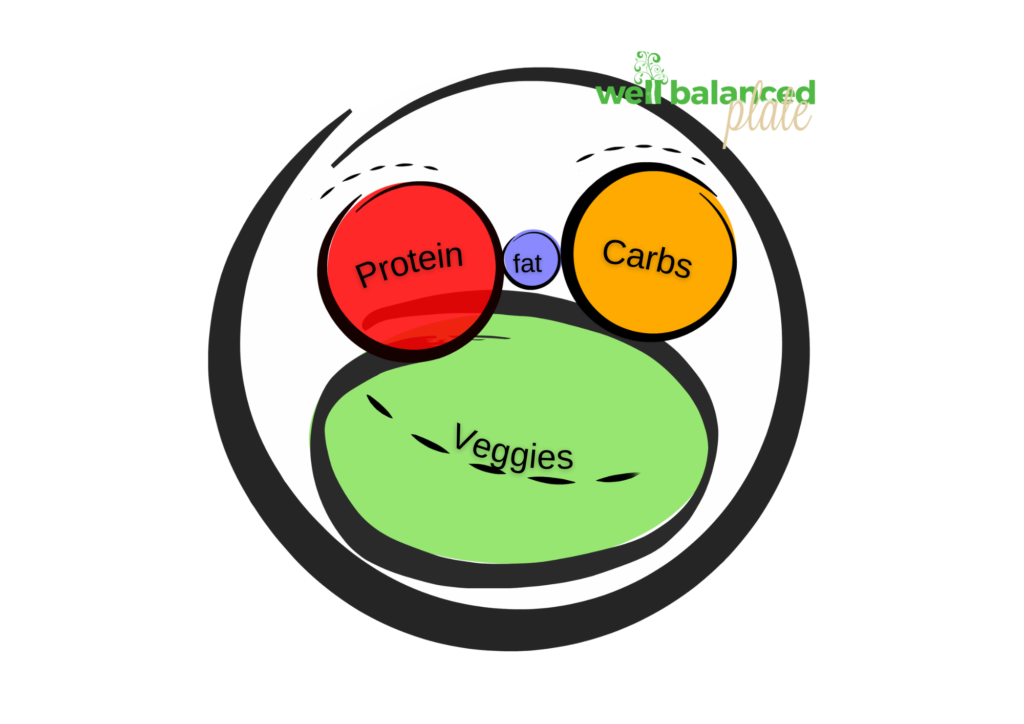
Build a PCOS-Friendly Plate:
To follow a balanced, anti-inflammatory meal plan, think of each meal including the following:
- ½ plate of non-starchy vegetables, the more colors the better
- ¼ plate of whole grains, starchy veggies (like quinoa or sweet potatoes), or whole/fresh fruit
- ¼ plate of lean proteins (chicken, tofu, fish, beans)
- + healthy fats like avocado, olive oil, nuts, or seeds
Why it works? Using the Well Balanced plate to build a meal ensures you are getting the right proportions of macronutrients to fight cravings, support gut health, limit blood sugar spikes, and fight inflammation.
Focus on Foods That Fight Inflammation
Certain foods can help calm inflammation in the body and support hormone balance and metabolic health. Try to include:
- Berries, leafy greens, broccoli, and bell peppers – these are rich in antioxidants and phytochemicals
- Fatty fish like salmon, sardines, and mackerel – high in omega-3 fatty acids
- Nuts and seeds like walnuts, flaxseeds, and chia seeds – healthy fats and antioxidants
- Fermented foods like yogurt, kefir, sauerkraut, and kimchi – support gut health and as result can reduce inflammation throughout the body
- Herbs and spices such as turmeric, ginger, and cinnamon have been shown to block inflammatory pathways and reduce the production of pro-inflammatory chemicals in the body.

What not to eat with PCOS
While we believe that restricting or eliminating food is not ideal, it’s hard to deny that reducing added sugars and ultra-processed foods can help you manage your PCOS. In the Well Balanced approach, we encourage you to be selective with your favorite sweet treats rather than avoid them altogether. Enjoying fun treats on occasion, without guilt or strict rules, and finding tasty, healthier alternatives will keep you from feeling deprived.
How refined sugars can make PCOS symptoms worse.
Understanding how foods high in refined sugars can make you feel worse, like triggering cravings, energy crashes, or mood swings, can help you make more informed and intentional choices.
Let’s say you enjoy a sweet treat, like a donut or soda. Here’s what happens in your body:
- It quickly breaks down into glucose (sugar), which floods your bloodstream and causes a sharp spike in blood sugar.
- In response, your pancreas releases insulin, which helps move glucose into your cells for energy.
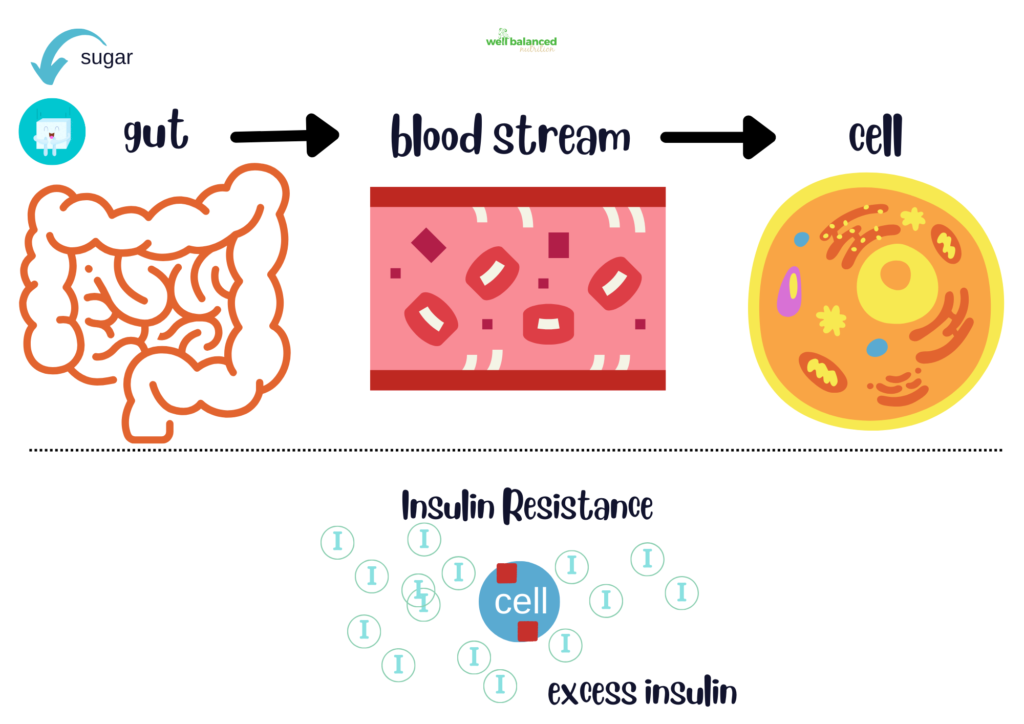
- But with insulin resistance, your cells don’t respond well to insulin’s signal. So the sugar stays in your blood, and your body produces even more insulin to try to fix the problem.
- Since the glucose isn’t used efficiently, your body stores the excess as fat, often around your midsection. This can make insulin resistance worse.
- On top of that, too much insulin can trigger higher androgen (male hormone) levels, which may lead to more acne, irregular periods, and stubborn weight gain.
If you want a personalized and more detailed nutrition plan based on your health, lifestyle, and goals, connect with our team at Well Balanced Nutrition to get started on a plan that truly works for you.
Lifestyle Strategies for Managing PCOS
Food is not the only thing that can affect insulin resistance, inflammation, and trigger more unwanted symptoms. Lifestyle behaviors and habits like movement, sleep, and stress management are also impactful tools to manage your PCOS symptoms.
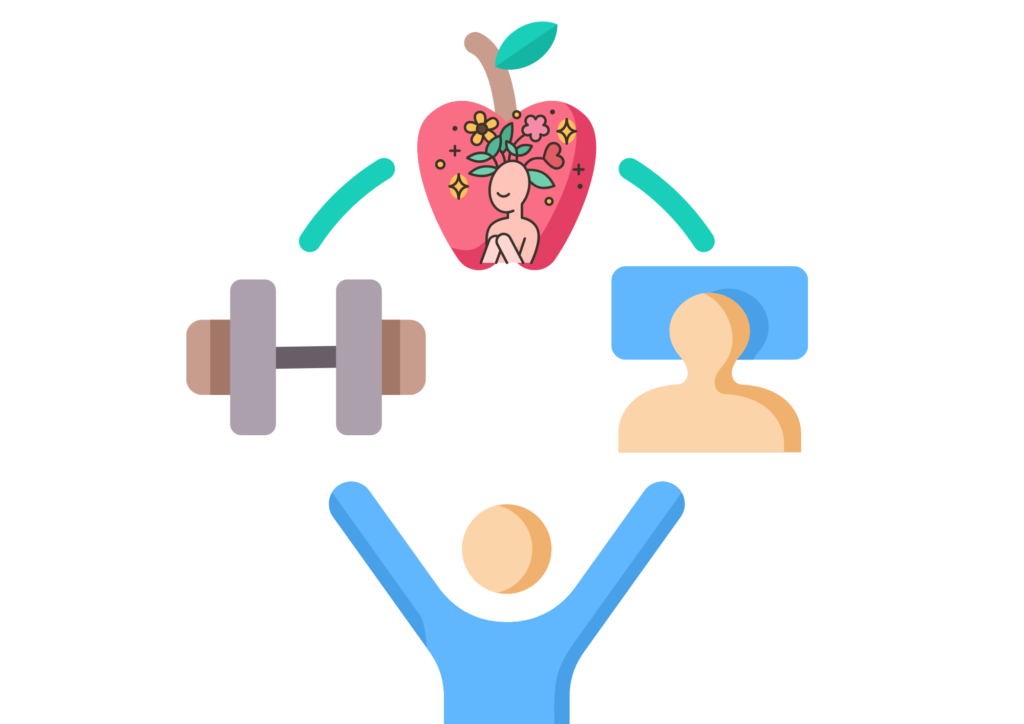
Move More: Exercise Helps Your Cells Listen to Insulin
When you move your body, your muscles use glucose for energy, which helps lower blood sugar levels. Even more importantly, exercise makes your cells more sensitive to insulin, so your body doesn’t have to work as hard to keep blood sugar in check.
Here’s how movement helps:
- Aerobic exercise (like walking, cycling, or swimming) improves how your body uses insulin during and after movement.
- Strength training (like lifting weights or bodyweight exercises) builds muscle, and the more muscle, the better your body can store and use glucose efficiently.
- Consistency matters more than intensity. You don’t need to go all-out every day—a brisk walk or dance session counts!
Prioritize Sleep: A Secret Weapon for Hormone Balance
Sleep isn’t just about rest—it plays a direct role in blood sugar regulation and hormone production. Poor or irregular sleep can increase insulin resistance, making PCOS symptoms worse.
Here’s what happens with poor sleep:
- Your body becomes less sensitive to insulin, leading to higher blood sugar and insulin levels.
- Appetite-regulating hormones (like leptin and ghrelin) get thrown off, increasing cravings, especially for sugary or high-carb foods.
- Inflammation increases, which may worsen symptoms like acne and fatigue.
Tips for better sleep:
- Aim for 7–9 hours of quality sleep each night.
- Stick to a consistent sleep schedule—even on weekends.
- Wind down with calming activities like reading, stretching, or a warm shower.
- Reduce screen time an hour before bed to protect melatonin production.
Manage Stress: Cortisol and Insulin Resistance
Chronic stress raises levels of cortisol, your body’s main stress hormone. While cortisol is helpful in short bursts, prolonged stress keeps it elevated, and that’s a problem for insulin resistance.
When cortisol stays high:
- It signals your liver to release more glucose into the bloodstream (a survival mechanism).
- It makes your cells more resistant to insulin.
- It encourages fat storage, especially around the midsection, which is linked to worse insulin resistance.
Stress reduction strategies we love:
- Deep breathing or meditation—even just 5 minutes a day
- Walking in nature or relaxing outside
- Creative outlets like journaling, music, or art
- Talking with a friend, coach, or therapist

Final Thoughts
There’s no quick fix for PCOS, but by making sustainable changes to how you eat, move, rest, and care for yourself, you can feel better in your body and mind. If you’d like a supportive partner to guide you through it all, our team at Well Balanced Nutrition is here to help. BOOK A FREE CLARITY CALL TO GET STARTED.



